Imagine a patient struggling to breathe, their chest heaving with each labored gasp. This is the reality for many individuals experiencing respiratory failure, a life-threatening condition where the lungs can’t adequately deliver oxygen to the body. Nursing care plays a vital role in managing this complex and critical situation, requiring a comprehensive approach to ensure patient safety and improve their chances of recovery.
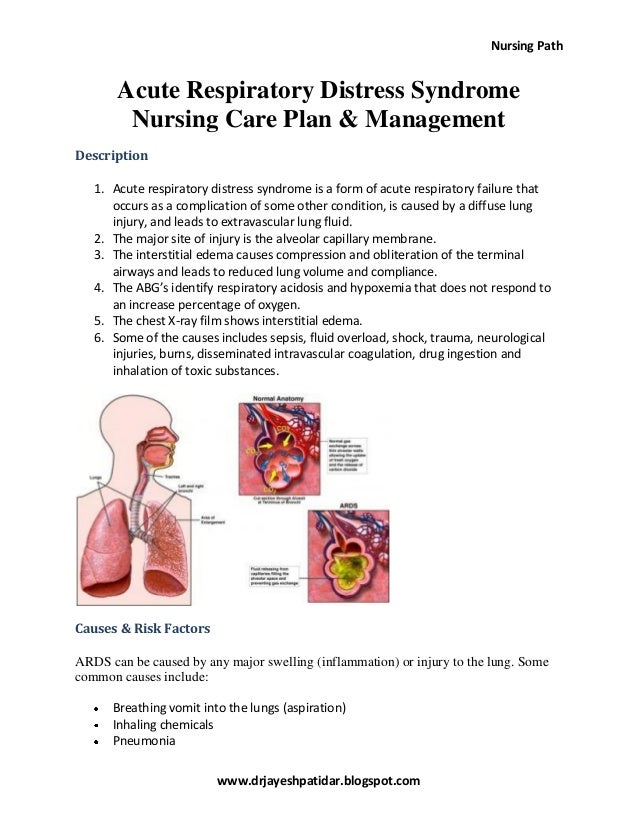
Image: imagetou.com
This article delves into the intricacies of a nursing care plan for patients with respiratory failure. We’ll explore the underlying causes, the crucial assessments, and the various interventions nurses use to stabilize patients and promote their well-being. Understanding this complex process will empower nurses to deliver effective care and provide comfort to patients navigating this challenging health crisis.
Understanding the Complexity of Respiratory Failure
Respiratory failure, a serious medical condition, occurs when the lungs are unable to provide the body with the oxygen it needs or remove enough carbon dioxide. Often a consequence of underlying disease or injury, it can be acute, developing rapidly, or chronic, developing gradually over time. The severity of respiratory failure is categorized based on the level of oxygen support required by the patient.
Types of Respiratory Failure
Respiratory failure can be classified into two main types:
- Hypoxemic respiratory failure: This type occurs when the lungs are unable to adequately transport oxygen into the bloodstream, leading to low blood oxygen levels (hypoxemia). Common causes include pneumonia, pulmonary embolism, and acute respiratory distress syndrome (ARDS).
- Hypercapnic respiratory failure: This type arises when the lungs fail to eliminate carbon dioxide effectively, leading to high carbon dioxide levels (hypercapnia) in the blood. It is often seen in patients with chronic obstructive pulmonary disease (COPD), neuromuscular disorders, and severe asthma.
A Comprehensive Nursing Care Plan
A well-crafted nursing care plan for patients with respiratory failure is paramount for ensuring their safety and promoting recovery. Here’s a breakdown of essential elements:
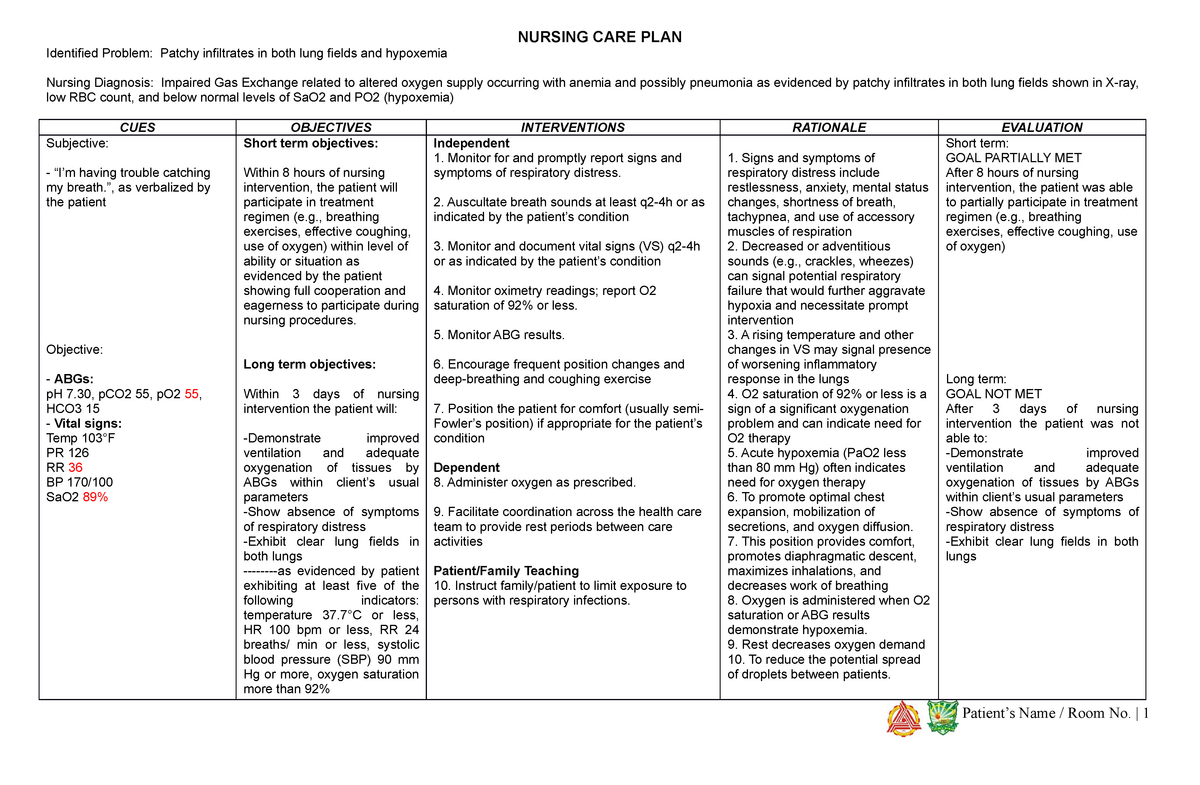
Image: www.studocu.com
1. Assessment and Monitoring
The first step involves a thorough assessment to determine the patient’s baseline status and identify any potential complications. Crucial assessments include:
- Respiratory assessment: This involves evaluating respiratory rate, effort, breath sounds, and oxygen saturation levels.
- Cardiovascular assessment: Monitoring vital signs like heart rate and blood pressure is also essential, as respiratory failure can impact cardiovascular function.
- Neurological assessment: Assessing level of consciousness and mentation is key, as changes in these domains can indicate worsening oxygenation or respiratory distress.
- Review of medical history and medications: Understanding the patient’s underlying illnesses and current medications is essential to guide appropriate interventions.
2. Maintaining an Open Airway
Ensuring an open and patent airway is essential for effective oxygen exchange. Nurses employ various techniques to maintain a clear airway:
- Positioning: Elevating the head of the bed and positioning the patient to maximize chest expansion can promote lung drainage and ease breathing.
- Suctioning: Regular suctioning of the airway is often necessary to remove secretions that can obstruct airflow.
- Endotracheal intubation: In cases of severe respiratory failure, intubation and mechanical ventilation may be required to assist the lungs in breathing.
3. Administering Oxygen and Ventilation
Providing supplemental oxygen is a cornerstone of respiratory failure management. The method and concentration of oxygen delivered depend on the severity of the patient’s condition.
- Nasal cannula: This low-flow method delivers oxygen through a nasal prongs and is suitable for mild cases.
- Face mask: Providing a higher oxygen flow, face masks come in various types, such as simple masks, partial rebreather masks, and non-rebreather masks.
- Mechanical ventilation: For critically ill patients with severe respiratory failure, non-invasive or invasive mechanical ventilation may be necessary to support respiration.
4. Managing Fluid Balance
Controlling fluid balance is crucial, as fluid overload can worsen respiratory distress. Nurses closely monitor fluid intake and output, and may adjust fluid administration as needed.
5. Providing Comfort and Psychological Support
Patients with respiratory failure often experience anxiety and fear, especially when experiencing respiratory distress. Providing emotional support and reassurance can help reduce anxiety and promote recovery.
- Empathy and communication: Nurses should engage in empathetic communication with patients, explaining procedures and responding to their concerns.
- Pain management: Effective pain management is critical, as pain can worsen respiratory effort and anxiety.
- Psychosocial support: Providing emotional support to patients and their families is vital, as respiratory failure can be a stressful and emotionally charged experience.
6. Monitoring for Complications
Nurses must vigilantly monitor for potential complications associated with respiratory failure, including:
- Pneumonia: Respiratory failure patients are prone to pneumonia, especially those on mechanical ventilation.
- Respiratory distress: Signs of worsening respiratory distress, such as increased work of breathing or changes in oxygenation, require immediate attention.
- Cardiac arrhythmias: Respiratory failure can affect heart rhythm. Nurses must monitor for any irregularities in heart rhythm.
- Ventilator-associated pneumonia: A serious complication that can develop in patients on mechanical ventilation.
7. Collaborating with the Healthcare Team
Effective management of respiratory failure requires a collaborative approach involving nurses, physicians, respiratory therapists, and other healthcare professionals.
Emerging Trends and Future Directions
The field of respiratory care is constantly evolving, with advancements in technology and therapeutic approaches. Here are some emerging trends:
- Non-invasive ventilation: Advancements in non-invasive ventilation techniques are expanding the options for managing respiratory failure, minimizing the need for intubation.
- Personalized medicine: Tailoring treatment plans based on individual patient characteristics, including genetic predisposition and response to medications, is becoming increasingly prevalent.
- Telehealth: The use of telehealth is increasing, enabling remote monitoring and consultation for patients with respiratory failure, improving accessibility and reducing hospitalization.
Nursing Care Plan For Patient With Respiratory Failure
Conclusion
Providing nursing care for patients with respiratory failure is a challenging yet rewarding endeavor. Nurses play a crucial role in stabilizing patients, improving their oxygenation, and promoting their well-being. By employing a comprehensive care plan that includes vigilant monitoring, effective interventions, and collaborative teamwork, nurses can make a significant difference in the lives of individuals facing this health crisis. As the field continues to evolve, nurses are at the forefront of providing evidence-based care and advocating for patient safety and optimal outcomes.



![Cyclomancy – The Secret of Psychic Power Control [PDF] Cyclomancy – The Secret of Psychic Power Control [PDF]](https://i3.wp.com/i.ebayimg.com/images/g/2OEAAOSwxehiulu5/s-l1600.jpg?w=740&resize=740,414&ssl=1)

