Every new mom cradles her precious baby, a tiny miracle born from nine months of anticipation and love. But those first few weeks after birth aren’t just about gazing at tiny toes and learning to breastfeed. They’re also a time when a woman’s body is working tirelessly to recover from the physical demands of labor and birth. An important part of that recovery is monitoring for potential complications, one of which is postpartum bleeding.

Image: www.pinterest.com
While most women experience a period of lighter bleeding known as lochia for several weeks after giving birth, some face a more serious risk of excessive bleeding, often called postpartum hemorrhage. This can happen to anyone, and it’s important to understand the signs and symptoms so you can get the proper support if needed.
Understanding The Risks: Postpartum Hemorrhage
Postpartum hemorrhage occurs when a woman loses more than 500 ml of blood after vaginal delivery or more than 1000 ml after a Cesarean section. This can be a life-threatening condition, but luckily, with proper care and monitoring, most cases are manageable.
Causes of Postpartum Hemorrhage
There are several factors that can contribute to postpartum hemorrhage, including:
- Uterine Atony: This is the most common cause of postpartum hemorrhage and occurs when the uterus doesn’t contract properly after delivery, leading to excessive bleeding.
- Lacerations: Tears in the cervix, vagina, or perineum (the area between the vagina and anus) can result in significant blood loss.
- Placenta Previa or Abruptio Placentae: These conditions, where the placenta is positioned abnormally or separates from the uterine wall before birth, can lead to heavy bleeding.
- Retained Placenta: If the placenta doesn’t detach from the uterine wall after birth, it can cause excessive bleeding.
- Blood Clotting Disorders: Some women have conditions that make it difficult for their blood to clot properly, increasing their risk of hemorrhage.
The Importance of Monitoring and Early Intervention
The key to handling postpartum hemorrhage lies in early detection and intervention. Hospitals have a system in place to monitor and assess the mother’s condition closely in the first few hours after delivery. This includes:
- Regularly Checking Vital Signs: A nurse will regularly assess a new mom’s blood pressure, heart rate, and temperature. Any significant changes could signal a problem.
- Evaluating Bleeding: The amount and color of the blood flow are carefully assessed. Lochia, the postpartum discharge, should gradually change from bright red to a darker brown. A sudden increase in the volume of bleeding or a return to bright red bleeding can be concerning.
- Palpating the Uterus: A nurse will feel the uterus to ensure it is firm and contracted. A soft or boggy uterus can indicate uterine atony, raising the risk of hemorrhage.
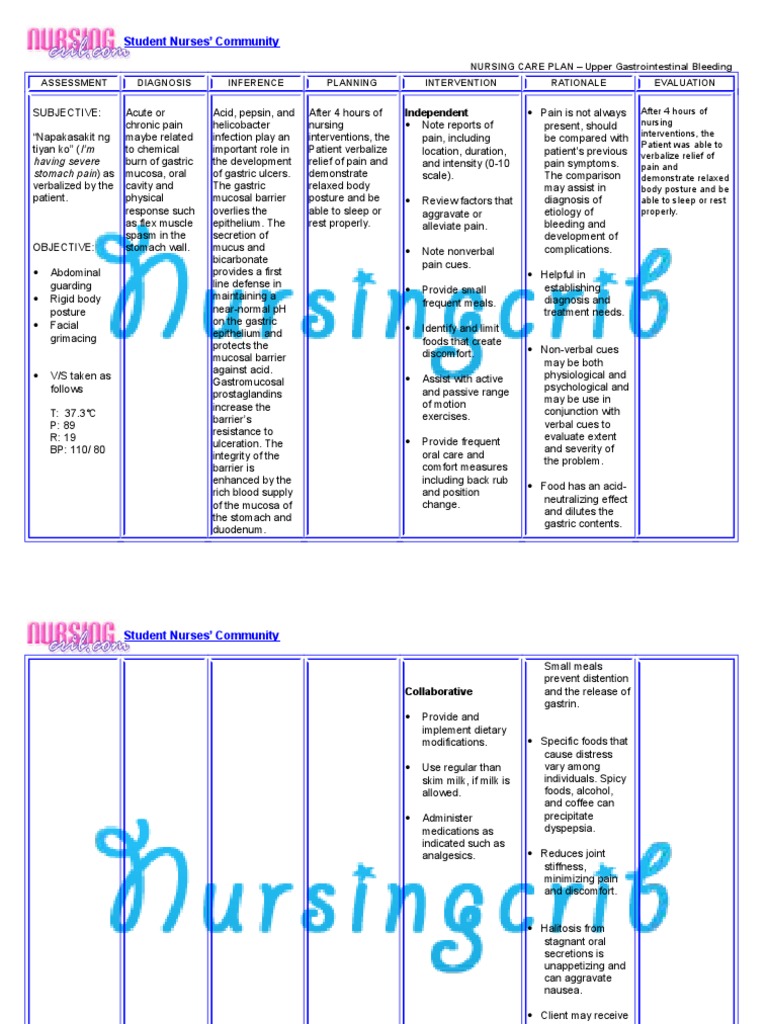
Image: www.scribd.com
The Nursing Care Plan: Managing Postpartum Bleeding
Nursing care for a postpartum woman at high risk for bleeding focuses on preventing and managing hemorrhage. The plan might include:
1. Immediate Measures:
- Fundal Massage: Nurses gently massage the uterus to encourage contractions and reduce bleeding.
- Uterine Medications: If fundal massage isn’t enough, medications like oxytocin or methylergonovine are administered to help the uterus contract and control bleeding.
- Bimanual Compression: In some cases, a nurse will apply pressure to the uterus both internally and externally to help stop the bleeding.
- Fluid Replacement: Intravenous (IV) fluids are often given to restore blood volume and prevent dehydration, particularly if there’s significant blood loss.
2. Continuous Monitoring:
- Observation of vital signs: Nurses will carefully monitor the mother’s heart rate, blood pressure, oxygen saturation, and respirations for any signs of instability.
- Assessing bleeding: The amount, color, and consistency of lochia are monitored regularly to identify any changes that could indicate a problem.
- Monitoring Urine Output: Reduced urine output can be a sign of dehydration or shock, both potential complications of postpartum hemorrhage.
3. Addressing Underlying Causes:
- Surgical Intervention: In cases of retained placenta, lacerations, or other complications, surgical procedures might be necessary to control bleeding.
- Blood Transfusions: If a woman has lost a significant amount of blood, a blood transfusion may be required to replenish lost red blood cells.
- Monitoring for Complications: Nurses keep a close eye on the mother for signs of infection, anemia, and other complications that could arise after a hemorrhage.
The Emotional Impact of Postpartum Hemorrhage
It’s crucial to remember that postpartum hemorrhage isn’t just a physical concern. It can also have significant emotional and psychological effects for the mother. The experience can be frightening, leaving a woman feeling vulnerable and anxious about her health and well-being.
Here’s what nurses can do to provide emotional support:
- Be empathetic and understanding: Acknowledge the woman’s fears and concerns and offer reassurance that she’s getting the best possible care.
- Stay informed about her recovery: Keep her informed about her progress and the next steps in her treatment.
- Provide information and resources: Give her reliable information about postpartum hemorrhage, its causes, and treatment options. Provide her with contacts for support groups and organizations that can offer emotional support and counseling.
- Advocate for her needs: If a mother is struggling to cope with the emotional impact of hemorrhage, advocate for her to receive appropriate psychological support and therapy.
Risk For Bleeding Nursing Care Plan Postpartum
Promoting a Safe and Healthy Postpartum Period
Postpartum hemorrhage is a serious condition, but with careful monitoring and immediate intervention, most women make a full recovery.
To promote a safe and healthy postpartum experience, women can:
- Discuss their individual risk factors with their healthcare provider: Talk to your doctor about any potential risk factors for postpartum hemorrhage, including previous births, medical conditions, and medications.
- Attend prenatal classes and learn about the signs and symptoms: Empowering yourself with knowledge is crucial.
- Follow your healthcare provider’s instructions carefully: Attend all your prenatal appointments, follow your doctor’s advice, and don’t hesitate to reach out with any concerns.
By working together, healthcare providers and new mothers can navigate the postpartum period with confidence, knowing that they have the knowledge and support to manage any potential complications. This includes the crucial role of nurses, who act as vital advocates and supporters throughout this vulnerable and transformative time.



![Cyclomancy – The Secret of Psychic Power Control [PDF] Cyclomancy – The Secret of Psychic Power Control [PDF]](https://i3.wp.com/i.ebayimg.com/images/g/2OEAAOSwxehiulu5/s-l1600.jpg?w=740&resize=740,414&ssl=1)

