The birth of a child is a moment of joy and celebration. However, for some mothers, this experience can be overshadowed by a potentially life-threatening complication: postpartum hemorrhage (PPH). PPH is defined as the loss of more than 500 ml of blood after vaginal delivery or more than 1000 ml after a cesarean section. It can occur rapidly or gradually and is a leading cause of maternal mortality worldwide. As a nurse, I have seen firsthand the devastating impact PPH can have on both mothers and families. This article aims to provide a comprehensive understanding of PPH, its risk factors, and the nursing care plan essential for managing this critical condition.
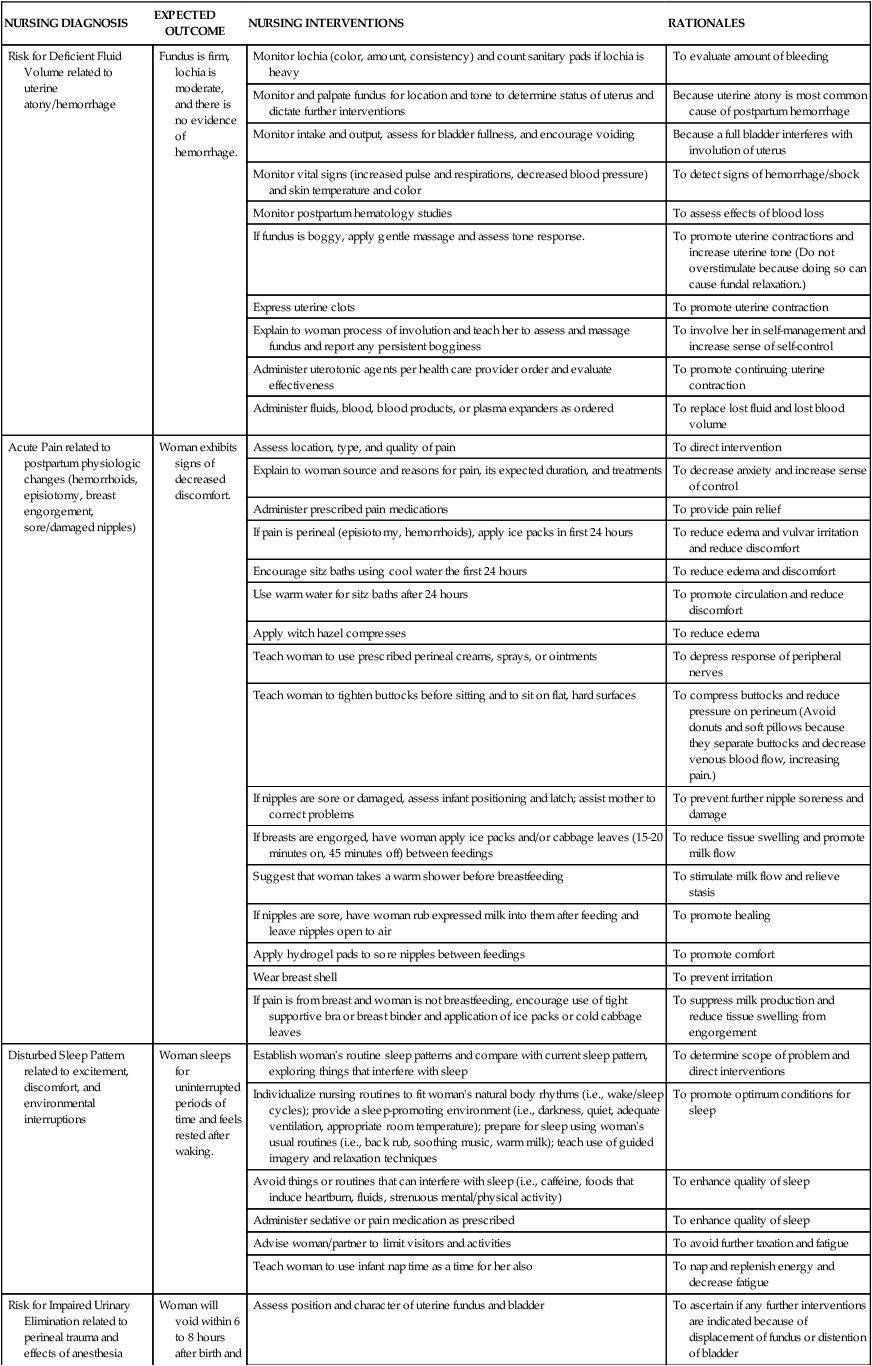
Image: www.hotzxgirl.com
Understanding the nursing care plan for PPH is crucial for ensuring timely intervention and optimal patient care. This article will delve into the intricacies of this plan, outlining the essential steps nurses take to stabilize the patient, prevent further blood loss, and promote recovery. By equipping nurses with the knowledge and skills to effectively manage PPH, we can contribute to improving maternal health outcomes and ensuring mothers can embrace their new role with confidence and well-being.
Understanding Postpartum Hemorrhage
Definition and Causes
Postpartum hemorrhage (PPH) is a significant complication of childbirth characterized by excessive blood loss following delivery. It can occur both after vaginal and cesarean deliveries. While PPH can be caused by various factors, some of the most common reasons include:
- Uterine atony: The most common cause of PPH, uterine atony, occurs when the uterus fails to contract properly after delivery, leading to excessive bleeding from the placental site.
- Retained placental fragments: When parts of the placenta remain in the uterus after delivery, it can prevent the uterus from contracting effectively, leading to hemorrhage.
- Lacerations: Tears in the cervix, vagina, or perineum during delivery can cause significant bleeding.
- Uterine rupture: A rare but serious complication, uterine rupture occurs when the uterus tears, resulting in significant bleeding into the abdominal cavity.
- Placenta previa or abruption: These conditions, where the placenta is abnormally positioned or detaches prematurely from the uterine wall, can lead to significant bleeding during pregnancy and delivery.
Risk Factors of Postpartum Hemorrhage
Several factors can increase a woman’s risk of developing PPH. These risk factors include:
- Previous PPH: Women who have experienced PPH in a previous pregnancy are at higher risk for reoccurrence.
- Multiple pregnancies: Women who have had multiple pregnancies are at increased risk due to uterine muscle stretching.
- Prolonged labor: Labor lasting longer than 12 hours increases the risk of uterine atony.
- Large baby: Babies weighing over 8 pounds are linked to an increased risk of PPH due to stretching of the uterus.
- Use of certain medications: Certain medications, including magnesium sulfate, can interfere with uterine contractions and increase the risk of PPH.
- Pre-existing medical conditions: Certain medical conditions, such as diabetes, hypertension, and clotting disorders, can increase the risk of PPH.
Image: nurseslabs.com
Classification of Postpartum Hemorrhage
Postpartum hemorrhage is classified based on the amount of blood loss. The classification provides a framework for understanding the severity of the hemorrhage and guiding treatment.
Early Postpartum Hemorrhage: Occurs within 24 hours of delivery.
Late Postpartum Hemorrhage: Occurs after 24 hours but within six weeks of delivery.
Understanding the classifications of PPH is crucial for recognizing the severity of the condition early and initiating appropriate interventions.
A Comprehensive Nursing Care Plan for Postpartum Hemorrhage
Effective management of PPH requires a well-defined nursing care plan tailored to the specific needs of the patient. The following outlines essential components of this plan:
1. Initial Assessment and Monitoring
Nurses play a critical role in the timely identification of PPH. The following assessment and monitoring strategies are essential:
- Vital signs: Closely monitor the patient’s vital signs, particularly pulse rate, blood pressure, and respiratory rate. A rapid pulse and low blood pressure can indicate significant blood loss.
- Blood loss estimation: Accurately estimate the amount of blood loss through visual inspection of perineal pads, counting them, and observing the consistency and color of the blood.
- Uterine assessment: Palpate the uterus to assess its firmness, position, and tenderness. A boggy, poorly contracted uterus suggests uterine atony.
- Vaginal examination: Perform a vaginal examination to assess for any lacerations or retained placental fragments.
- Laboratory tests: Monitor hemoglobin and hematocrit levels to assess the severity of blood loss.
2. Immediate Interventions to Control Bleeding
Prompt interventions are critical to control bleeding and prevent further blood loss:
- Fundal massage: Start gentle fundal massage to encourage uterine contraction and reduce bleeding.
- Uterine packing: In cases of persistent bleeding despite fundal massage, uterine packing with gauze may be used to help compress the bleeding vessels.
- Fluid resuscitation: Administer intravenous fluids to restore blood volume and maintain hemodynamic stability.
- Blood transfusions: In cases of severe blood loss, blood transfusions may be necessary to replace lost blood and maintain adequate oxygen-carrying capacity.
3. Pharmacological Interventions
Medication plays a crucial role in managing PPH:
- Uterotonic medications: Uterotonic agents, such as oxytocin, methylergonovine, and carboprost, stimulate uterine contractions to reduce bleeding.
- Antibiotics: Prophylactic antibiotics may be administered to prevent infection, particularly after procedures such as uterine packing.
4. Surgical Interventions
In some cases, surgical interventions are necessary to control PPH.
- Dilation and curettage (D&C): If retained placental fragments are the cause of bleeding, D&C may be performed to remove them.
- Embolization: In some cases, embolization of the uterine arteries may be performed to stop bleeding.
- Hysterectomy: In severe cases of PPH, a hysterectomy may be necessary to control bleeding and save the patient’s life.
5. Psychologic Support for the Patient
The experience of PPH can be very stressful for the patient. Nurses should provide psychological support and emotional assistance during this challenging time.
- Communicate effectively: Communicate clearly and honestly with the patient about their condition, treatment plan, and prognosis.
- Empathy and reassurance: Provide empathy and reassurance, acknowledging the patient’s emotions and fears.
- Involve the family: Encourage family members to participate in the patient’s care and provide emotional support.
Tips and Expert Advice for Managing Postpartum Hemorrhage
Effective management of PPH requires a combination of knowledge, skills, and a proactive approach. Here are some tips and expert advice for nurses:
Early Recognition is Key: Be vigilant in monitoring the postpartum patient for signs and symptoms of PPH. Even small changes in vital signs or blood loss can indicate early stages of this complication.
Prepare for Emergencies: Ensure readiness for PPH by keeping emergency equipment like uterine packing, uterotonic medications, and blood transfusion supplies readily available. Conduct regular drills and simulations to ensure proficiency in managing PPH emergencies.
Collaborate Effectively: Work closely with the physician and other healthcare professionals to ensure coordinated care. Open communication between team members is vital for prompt interventions and successful management.
Remain Calm and Confident: Maintaining composure and a calm demeanor amidst a PPH emergency is vital. Effective leadership and clear communication help to keep the team focused and ensure optimal patient care.
FAQ’s
Q: What are the immediate signs and symptoms of PPH?
A: The most common signs and symptoms of PPH include:
- Rapid pulse
- Low blood pressure
- Pale skin
- Lightheadedness or dizziness
- Excessive vaginal bleeding
- Uterine tenderness or bogginess (feeling soft and spongy)
Q: What measures can I take to reduce my risk of PPH?
A: There are several steps you can take to reduce your risk of PPH:
- Receive prenatal care throughout pregnancy.
- Maintain a healthy weight gain during pregnancy.
- Discuss any pre-existing medical conditions with your doctor.
- Avoid smoking or using illegal drugs.
- Attend childbirth education classes to learn about common postpartum complications.
Q: Why is PPH a major concern for maternal health?
A: PPH is a serious health threat for mothers because it can lead to various complications, including:
- Hypovolemic shock: Significant blood loss can lead to a decrease in blood volume, causing shock and potentially organ damage.
- Anemia: PPH can cause anemia, a condition characterized by a lack of red blood cells, leading to fatigue, weakness, and shortness of breath.
- Blood clots: In some cases, PPH can trigger blood clots, which can travel to the lungs or other organs, causing serious complications.
- Death: Untreated PPH can be fatal, making it a leading cause of maternal mortality worldwide.
Nursing Care Plan For Postpartum Haemorrhage
Conclusion
Postpartum hemorrhage is a serious complication of childbirth that requires prompt recognition, timely intervention, and a well-coordinated nursing care plan. Nurses play a vital role in managing this condition, ensuring the safety and well-being of mothers. By understanding the risk factors, signs and symptoms, and essential components of the nursing care plan, nurses can proactively address PPH and contribute to improving maternal health outcomes.
Are you interested in learning more about the specific interventions and strategies used in managing postpartum hemorrhage? We invite you to share your thoughts and ask any questions you have in the comments section below.



![Cyclomancy – The Secret of Psychic Power Control [PDF] Cyclomancy – The Secret of Psychic Power Control [PDF]](https://i3.wp.com/i.ebayimg.com/images/g/2OEAAOSwxehiulu5/s-l1600.jpg?w=740&resize=740,414&ssl=1)

