Imagine struggling to breathe, feeling like your lungs are constantly weighed down with a heavy blanket. This is the daily reality for countless individuals living with Chronic Obstructive Pulmonary Disease (COPD). COPD is a progressive lung disease that makes it hard to breathe, and unfortunately, there is no cure. But what if you could learn how to manage your symptoms and live a fuller life?

Image: simple-decoratedhouse.blogspot.com
This comprehensive guide provides insights into the invaluable tool that is a nursing care plan for COPD. We’ll explore the essential elements of this plan, highlighting how it empowers individuals with COPD to take control of their well-being. Whether you’re a patient, a caregiver, or a healthcare professional, understanding how to effectively utilize a nursing care plan is vital. This guide will equip you with the knowledge to navigate the challenges of COPD and pave the way for better health and quality of life.
Understanding COPD: The Foundation for Care
COPD stems from long-term damage to the lungs, primarily caused by smoking. The constant exposure to irritants like cigarette smoke leads to chronic inflammation, eventually obstructing airflow and compromising lung function. This obstruction makes it difficult for the lungs to expel carbon dioxide and draw in adequate oxygen, resulting in breathlessness, wheezing, and other symptoms.
The Importance of a Nursing Care Plan
A nursing care plan for COPD is not just a document; it’s a customized roadmap for managing the disease effectively. It outlines a personalized strategy designed to address each individual’s unique needs and challenges. Think of it as a collaborative effort between the patient, their family, and healthcare professionals, working together to improve their quality of life.
Key Elements of a Nursing Care Plan for COPD
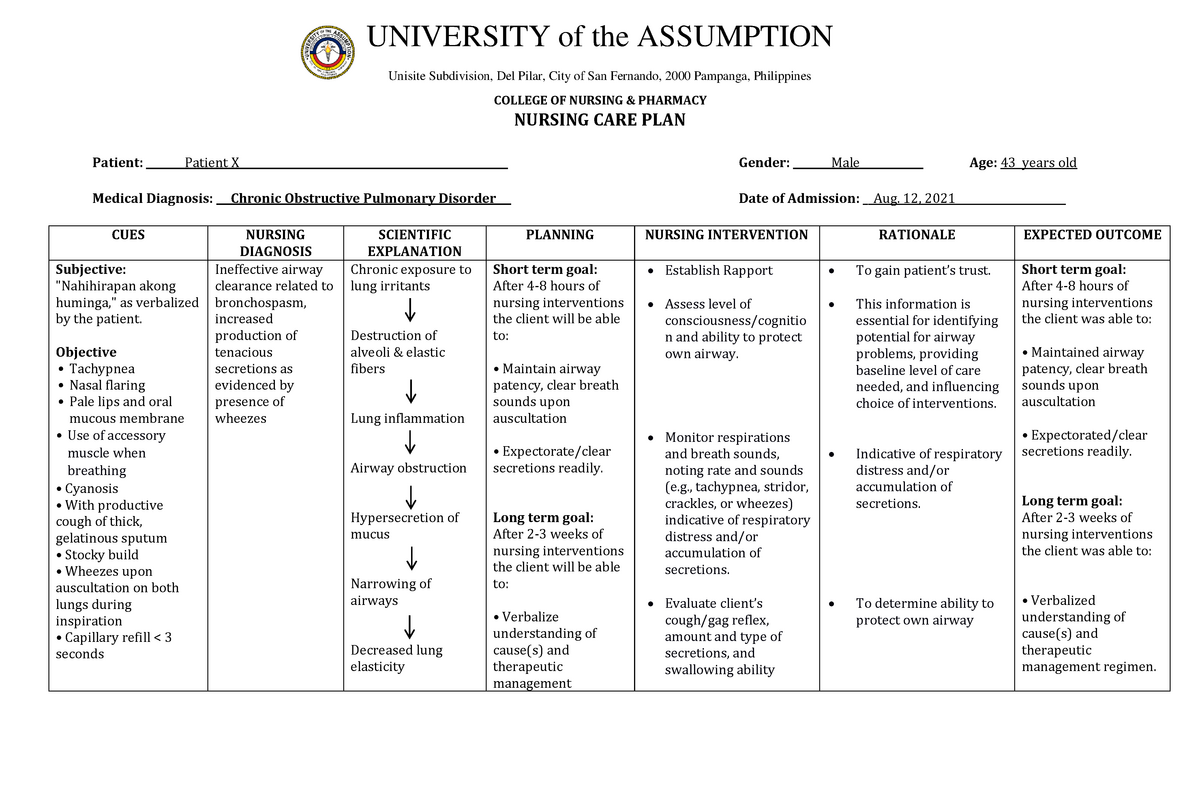
Image: www.studocu.com
1. Assessment: Defining the Patient’s Needs
The foundation of any effective care plan lies in a thorough assessment. This involves gathering essential information about the patient’s health history, current symptoms, lifestyle, and social support system. It’s like piecing together a puzzle to understand the individual’s complete picture.
- Medical History: Identifying past diagnoses, medications, and surgeries.
- Symptoms: Evaluating the severity and frequency of symptoms like shortness of breath, coughing, wheezing, and chest tightness.
- Functional Status: Assessing the patient’s ability to perform everyday activities like walking, bathing, and dressing. This helps determine the need for assistance.
- Social Support: Evaluating the availability of family, friends, or community resources to provide support and care.
2. Goals: Setting a Course for Improvement
Once the assessment is complete, the next step is to identify measurable and achievable goals that align with the patient’s individual needs and aspirations. These goals should be established collaboratively, ensuring they represent the patient’s wishes and priorities.
- Symptom Management: Aims to minimize the severity and frequency of COPD symptoms. Examples include reducing shortness of breath, improving breathing capacity, and reducing coughing.
- Functional Improvement: Focuses on enhancing the patient’s ability to perform daily activities, leading to greater independence.
- Education and Empowerment: Equipping the patient with the knowledge and skills to understand and manage their condition effectively.
- Emotional Support: Addressing the emotional impact of COPD, including anxiety, depression, and social isolation.
3. Interventions: Tools for a Better Life
Interventions are the specific actions that nurses and other healthcare professionals take to achieve the established goals. They’re the practical steps that translate the plan into real-world improvement. These interventions can be tailored to encompass a wide range of therapies and techniques.
- Medications: Inhalers, bronchodilators, and corticosteroids are essential in managing COPD symptoms. Proper medication usage is crucial, and the nursing care plan will outline dosage, timing, and any potential side effects.
- Oxygen Therapy: For patients with severe COPD, supplemental oxygen can significantly improve breathing and daily functioning. This may be required at home or during specific activities.
- Breathing Exercises: Pursed-lip breathing, diaphragmatic breathing, and controlled breathing techniques can help improve airflow, reduce shortness of breath, and enhance lung capacity. The nursing care plan will specify correct techniques and appropriate frequencies.
- Pulmonary Rehabilitation: This structured program often combines exercise, education, and counseling to improve lung function, muscular strength, and stamina, allowing individuals to manage daily activities more effectively.
- Lifestyle Modifications: Quitting smoking, avoiding irritants like dust and fumes, and adopting a healthy diet and exercise routine are crucial for managing COPD. The nursing care plan will provide tailored guidance on reducing exposure to these triggers and making positive lifestyle changes.
- Emotional Support and Counseling: Living with a chronic illness like COPD can be emotionally challenging. The nursing care plan may include referrals to support groups, counseling, or mental health services to address anxiety, depression, and feelings of isolation.
4. Monitoring and Evaluation: Tracking Progress
The nursing care plan is not a rigid set of instructions but rather a dynamic framework that evolves alongside the patient’s needs. Regular monitoring and evaluation are crucial to ensure that the plan remains relevant and effective. This involves tracking the patient’s progress, identifying any potential issues or roadblocks, and making necessary adjustments along the way.
- Symptom Monitoring: Regularly assessing the frequency and severity of COPD symptoms. This may involve using a symptom diary or employing devices like peak flow meters to track airflow.
- Functional Assessment: Periodically evaluating the patient’s ability to perform daily tasks and identifying any areas where additional support or adaptive strategies may be needed.
- Medication Effectiveness: Monitoring the effectiveness of medications, making adjustments to dosage or type as necessary to optimize symptom management.
- Patient Satisfaction: Genuinely understanding how the patient feels about their care plan and ensuring their needs and priorities are being addressed.
The Benefits of Utilizing a Nursing Care Plan for COPD
Implementing a comprehensive nursing care plan for COPD offers a multitude of benefits. It goes beyond simply managing symptoms; it empowers individuals to take control of their health and well-being, improving their overall quality of life.
- Reduced Symptoms: Effective symptom management, leading to less shortness of breath, less wheezing, and improved breathing capacity. This can significantly enhance daily life and decrease the need for emergency care.
- Increased Functional Abilities: Improved physical fitness, enabling individuals to participate in activities they enjoy and maintain their independence. This can span from simple tasks like getting dressed to more demanding activities like gardening or walking.
- Enhanced Quality of Life: A greater sense of control and confidence in managing COPD, leading to improved mental health and a more positive outlook on life. This can empower individuals to live fulfilling lives and participate fully in activities they cherish.
- Improved Overall Health: Reduced risk of complications, hospitalizations, and other health problems associated with COPD. By proactively managing the disease, individuals can minimize its impact on their overall health and well-being.
- Increased Patient Satisfaction: Improved communication and understanding between patients and healthcare providers, leading to greater trust, empowerment, and a more positive experience with the healthcare system.
How to Access a Nursing Care Plan for COPD
The beauty of a nursing care plan for COPD lies in its personalized nature. To access one, you need to be involved in the process. Reach out to your healthcare provider, schedule an appointment, and express your desire to create a customized care plan. The process typically involves a comprehensive assessment, followed by discussions with your healthcare team to establish goals and interventions that align with your specific needs.
If you’re looking for a template, or examples to guide you, a quick online search for “nursing care plan for COPD” can yield several PDFs, including templates that can be adapted. Remember, these PDFs are just guides and should be used in conjunction with the personalized care plan you create with your doctor and nurse.
Nursing Care Plan For Copd Pdf
Conclusion
Living with COPD doesn’t have to mean living a limited life. A nursing care plan is a powerful tool that can make a world of difference. By embracing its principles, individuals with COPD can gain control of their symptoms, improve their quality of life, and navigate the challenges of this disease with greater confidence. Remember, your health journey is unique, so work closely with your healthcare team to create a plan that’s right for you. Take the first step today, and unlock a brighter future with COPD.



![Cyclomancy – The Secret of Psychic Power Control [PDF] Cyclomancy – The Secret of Psychic Power Control [PDF]](https://i3.wp.com/i.ebayimg.com/images/g/2OEAAOSwxehiulu5/s-l1600.jpg?w=740&resize=740,414&ssl=1)

