You’re rushing to make it to the bathroom, but instead of the relief you seek, you’re met with a frustrating blockage. Sounds familiar? Constipation, a common ailment, affects people of all ages and can be a source of discomfort and distress. But fear not! With the right knowledge and a tailored approach, you can overcome this uncomfortable challenge.

Image: www.vrogue.co
This article delves into the critical role of nurses in managing constipation. We’ll explore the fundamentals of constipation, understand the different types, and delve into a step-by-step nursing care plan designed to address this common ailment. Whether you’re a healthcare professional looking to enhance your skills or simply seeking useful information, this comprehensive guide will empower you to better navigate this common health concern.
Understanding the Basics: What is Constipation?
Constipation is a condition characterized by infrequent bowel movements, difficulty passing stool, or the passage of hard, dry stools. It’s not a disease itself, but rather a symptom that can be caused by various factors. The frequency of bowel movements varies from person to person. Generally, a healthy individual passes stool at least 3 times a week, but some may have a daily bowel movement. A decrease in usual bowel frequency, accompanied by other symptoms, might indicate constipation.
Types of Constipation
Understanding the different types of constipation helps nurses tailor treatment and care effectively. Constipation is broadly categorized into two main types:
1. Primary Constipation:
Primary constipation describes cases where constipation is the main problem, with no underlying medical condition contributing to it. This type of constipation is often associated with lifestyle factors, such as diet, lack of exercise, and stress.
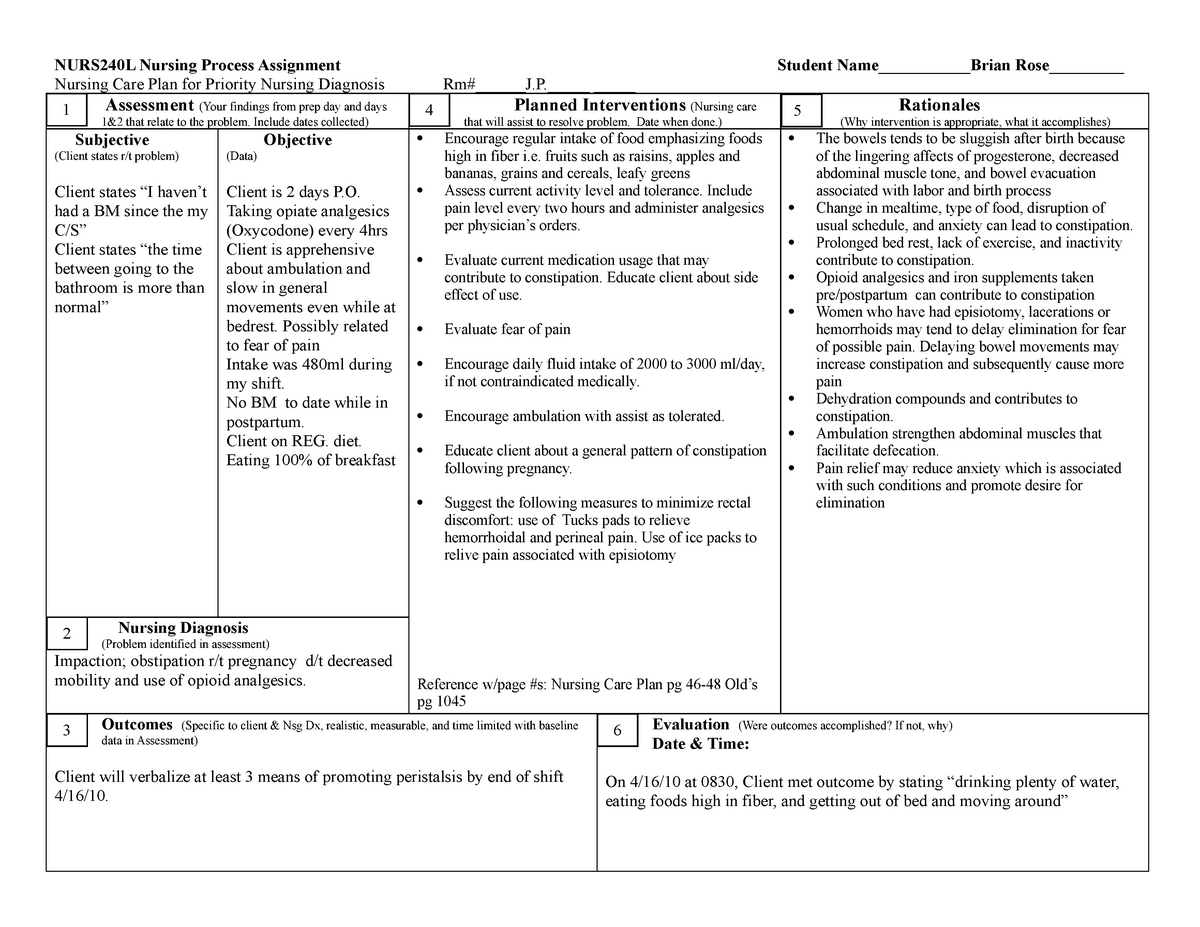
Image: www.aiophotoz.com
2. Secondary Constipation:
Secondary constipation occurs when an underlying medical condition triggers constipation. Many conditions can cause constipation, including:
- Hormonal imbalances: Thyroid disorders, diabetes, and hypothyroidism can affect bowel motility.
- Gastrointestinal disorders: Irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and diverticulitis can contribute to constipation.
- Medications: Various medications, including pain relievers (opioids), antidepressants, and anticonvulsants, can slow down bowel movements.
- Neurological conditions: Parkinson’s disease, multiple sclerosis, and stroke can impair nerve function, leading to constipation.
- Electrolyte imbalances: Dehydration, low levels of potassium or magnesium, or hypercalcemia can contribute to slow bowel movements.
- Structural abnormalities: Conditions affecting the intestines, such as anal fissures, hemorrhoids, and a narrowed colon, can make bowel movements painful and difficult.
The Importance of a Comprehensive Nursing Care Plan
A well-designed nursing care plan is crucial for effectively managing constipation. It serves as a roadmap, outlining individualized strategies to address the specific needs of the patient. A comprehensive care plan involves several key aspects:
Assessment: Gathering the Vital Clues
Before creating a care plan, it’s crucial for nurses to gather information about the patient’s history, symptoms, and lifestyle. This assessment process is vital to identify the underlying causes of constipation and personalize the care plan. Key aspects of the assessment include:
1. Patient History:
- Previous constipation episodes and their duration
- Previous medical conditions
- Current medications
- Family history of constipation
- Dietary habits and fluid intake
- Activity level
- Recent changes in lifestyle or bowel habits
2. Physical Examination:
- Abdominal examination: Check for distension, tenderness, bowel sounds, and masses.
- Rectal examination: Assess for fecal impaction, hemorrhoids, or other abnormalities.
3. Patient Interview:
- Symptoms: Frequency and characteristics of bowel movements, pain during defecation, straining, feeling of incomplete evacuation, bloating, abdominal pain, and any blood in the stool.
- Impact: Explore how constipation affects daily life, quality of sleep, social activities, and overall well-being.
- Lifestyle: Current diet, fluid intake, physical activity level, stress levels, and any recent travel or environmental changes.
Interventions: Targeting the Roots of Constipation
The interventions used in the nursing care plan aim to manage the underlying cause of constipation and provide relief to the patient. Effective interventions can include:
1. Diet and Fluid Intake:
- High-fiber diet: Encourage the consumption of fruits, vegetables, and whole grains. These foods add bulk to stool and stimulate bowel movements.
- Adequate hydration: Drinking plenty of water helps soften stool and promote easier passage. It’s recommended to drink at least 8 glasses of water per day.
- Avoidance of constipating foods: Limit intake of red meat, processed foods, dairy products, and sugary drinks, as these can worsen constipation.
2. Exercise:
- Regular physical activity: Aim for at least 30 minutes of moderate-intensity exercise most days of the week. Exercise stimulates bowel movements and helps regulate intestinal function.
- Positioning: Encourage patients to sit on the toilet in a relaxed position with their feet flat on the floor. This helps facilitate bowel movements.
3. Medications:
Depending on the severity and underlying cause of constipation, medication may be prescribed. Commonly used medications include:
- Laxatives: These medications act to soften stool and stimulate bowel movements. Laxatives come in various forms, including bulk-forming, osmotic, stimulant, and stool softeners.
- Antispasmodics: These medications relax the muscles of the intestinal tract to relieve cramping and pain.
- Stool softeners: These medications help soften stool, making it easier to pass.
4. Bowel Training:
For patients with chronic constipation, bowel training can be helpful. This involves establishing a regular bowel routine to train the digestive system to function more efficiently. Steps may include:
- Setting a regular time for bowel movements: Try to go to the bathroom at the same time each day, even if you don’t feel the urge.
- Creating a relaxed environment: Find a quiet and comfortable place to use the toilet.
- Allowing sufficient time: Don’t rush the process. Give yourself enough time to have a bowel movement.
- Using a footstool: Elevating your feet during bowel movements can help relax the pelvic muscles.
- Proper posture: Leaning forward slightly can help relieve pressure on the rectum.
5. Manual Disimpaction:
In cases of severe constipation or fecal impaction, manual disimpaction may be necessary. This procedure involves manually removing the impacted stool from the rectum. It’s usually performed by a healthcare professional and may involve the use of lubricants and gentle pressure.
Evaluation: Monitoring Progress and Adjusting the Plan
Regular evaluation is essential to ensure the effectiveness of the nursing care plan. Nurses should monitor the patient’s response to treatment and make necessary adjustments. Key aspects of evaluation include:
1. Frequency and consistency of bowel movements:
Assess the number of bowel movements per week and the consistency of the stool. Has the patient’s bowel frequency and stool consistency improved?
2. Symptom relief:
Evaluate whether the patient’s symptoms, such as abdominal pain, bloating, and straining, have been alleviated. Has the patient experienced a reduction in discomfort?
3. Response to interventions:
Assess the effectiveness of various interventions, including diet modifications, exercise, medications, and bowel training. Are any specific interventions proving more beneficial than others? Are there any adverse effects or intolerances to medications?
4. Overall well-being:
Evaluate the patient’s overall well-being, including their energy levels, mood, and quality of life. Has the patient experienced improvements in overall well-being since the implementation of the care plan?
Preventing Constipation: Embracing Lifestyle Changes
Preventing constipation involves proactive measures to maintain regular bowel function. These strategies include:
1. Establish Regular Bowel Habits:
Aim for a consistent bowel routine—going to the bathroom at the same time each day can help regulate bowel movements. Listen to your body and heed the call of nature!
2. Increase Fiber Intake:
Include plenty of high-fiber foods in your daily diet. These foods add bulk to stool and stimulate bowel contractions. High-fiber foods include fruits, vegetables, whole grains, and legumes.
3. Hydrate Adequately:
Drink plenty of fluids, especially water. Adequate hydration helps soften stool and facilitate easier passage.
4. Engage in Regular Exercise:
Physical activity stimulates bowel contractions and promotes regularity. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
5. Manage Stress:
Chronic stress can contribute to constipation. Practice stress-reducing techniques, such as exercise, yoga, meditation, or spending time in nature.
6. Limit Constipating Foods:
Reduce your intake of processed foods, red meat, dairy products, and sugary drinks. These foods can worsen constipation.
7. Consult a Healthcare Professional:
If you experience persistent constipation, consult a doctor or nurse for proper diagnosis and treatment. Underlying medical conditions might require specific interventions.
Example Of Nursing Care Plan For Constipation
Conclusion: Unclogging the Path to Relief
Constipation is a common but uncomfortable condition that can significantly impact quality of life. A comprehensive nursing care plan, tailored to the individual patient, is essential for effectively managing this condition. By understanding the different types of constipation, conducting thorough assessments, implementing appropriate interventions, and monitoring progress closely, nurses play a crucial role in restoring bowel regularity and improving patient well-being. Remember, prevention is key! Embrace lifestyle changes, such as a high-fiber diet, adequate hydration, regular exercise, and stress management techniques, to maintain optimal gut health and prevent constipation from disrupting your life.



![Cyclomancy – The Secret of Psychic Power Control [PDF] Cyclomancy – The Secret of Psychic Power Control [PDF]](https://i3.wp.com/i.ebayimg.com/images/g/2OEAAOSwxehiulu5/s-l1600.jpg?w=740&resize=740,414&ssl=1)

